The Ocular System: From Theory to Application in Clinical Neuroscience
Eye Movements as the Most Sensitive Biomarker of Brain Function
See the Brain Through the Eyes
Ocular motor control reveals the integrity of the entire neuroaxis — learn to read it with
clinical mastery. The eyes function as the most precise diagnostic instrument a manual
practitioner can possess, offering real-time insights into neurological function that
cannot be obtained through any other means.
They reveal cerebellar coordination, vestibular integration patterns, cortical activation
states, and hemispheric balance with extraordinary precision. Each movement, each
correction, each failure to stabilize gaze tells a story about the underlying neural
architecture supporting it.
Module 3 teaches you how to interpret ocular motor behavior with the sophistication of
a neurological specialist — and more importantly, how to translate that information into
actionable treatment strategies that produce measurable clinical outcomes.
Program Details
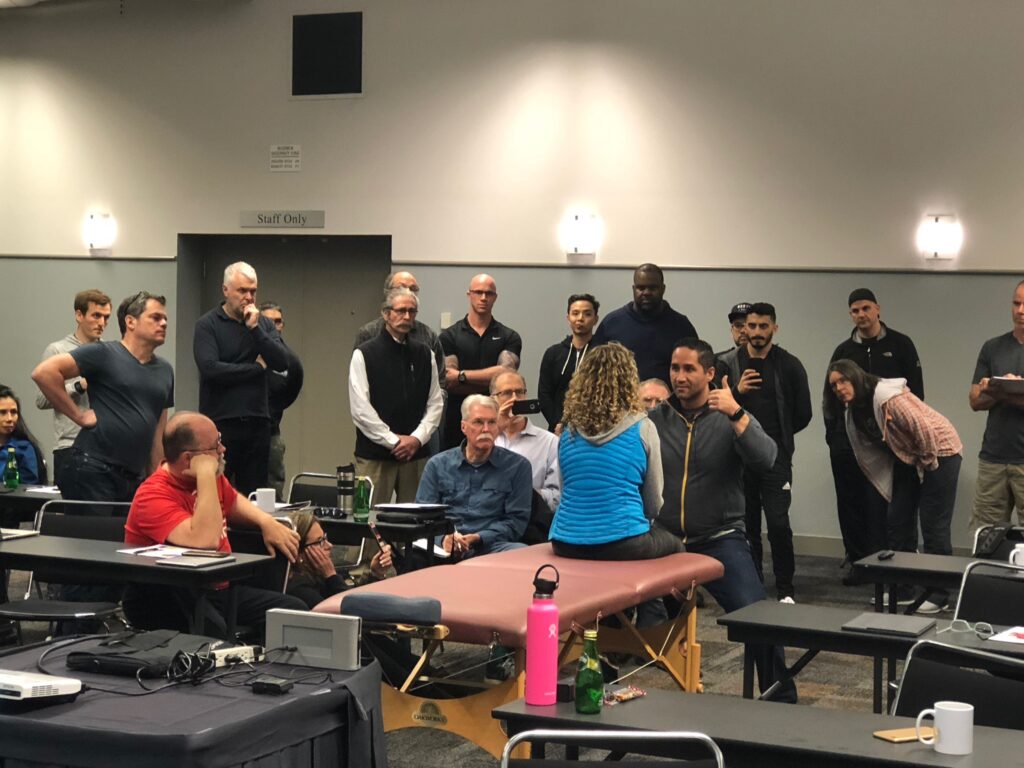
- 25 contact hours of advanced training
- Limited enrollment for optimal learning
- Hands-on clinical assessment protocols
- Certificate of completion included
The NeuroVirtus Promise
You will learn to evaluate the eyes not as isolated anatomical structures, but as a dynamic, integrated expression of global brain function. This
paradigm shift transforms how you understand neurological examination and creates new pathways for therapeutic intervention.
Our approach moves beyond simple screening tests to comprehensive understanding. You’ll develop the ability to observe subtle asymmetries,
interpret compensation patterns, and recognize the clinical significance of findings that others miss. This level of expertise separates advanced
practitioners from those using cookbook approaches.
By the end of this module, you will possess a skillset that rivals specialists who have trained for years in academic medical centers. You’ll be able to
communicate findings with precision, justify clinical decisions with confidence, and achieve outcomes that consistently exceed patient expectations.
Why This Module Matters

Post-Concussion
Syndrome
Ocular dysfunction is present in
over 90% of concussion cases.
Learn to identify and treat pursuit
deficits, convergence insufficiency,
and saccadic abnormalities that
perpetuate symptoms long after
injury.

Vestibular Disorders
Visual-vestibular mismatch drives
persistent dizziness and imbalance. Master the integration
between eye movements and
vestibular reflexes to resolve
chronic cases that haven’t
responded to traditional
approaches.

Chronic Pain Patterns
Abnormal ocular motor control
influences muscle tone, postural
alignment, and pain perception.
Discover how correcting eye
movement dysfunction can resolve treatment-resistant cervical and thoracic complaints.

Cognitive Fatigue
Inefficient eye movements create
excessive cognitive load, depleting
mental resources throughout the
day. Address the ocular
contributions to brain fog and
concentration difficulties in your
patients.
Ocular Anatomy & Neurophysiology
Understanding ocular motor function begins with mastery of the anatomical and neurophysiological substrate. This module provides comprehensive
coverage of the structures and circuits that enable precise eye movement control.
Peripheral Components
Central Control Networks
- Six extraocular muscles per eye and their biomechanical properties
- Cranial nerve innervation patterns (III, IV, VI)
- Neuromuscular junction physiology specific to ocular muscles
- Orbital mechanics and axis of rotation principles
- Brainstem gaze centers: PPRF, riMLF, and their connectivity
- Cerebellar modulation: flocculus, vermis, and fastigial nucleus
- Cortical control: frontal eye fields, parietal eye fields, supplementary eye fields
- Basal ganglia contributions to volitional saccades
Types of Eye Movements
The human ocular motor system employs five distinct movement categories, each serving specific visual and postural functions. Mastering their
evaluation requires understanding their unique neural substrates and functional purposes.
Smooth Pursuit
Tracking slow-moving objects
requires cerebellar-cortical
coordination. Pursuit deficits
indicate posterior fossa or
parietal dysfunction and commonly accompany
vestibular complaints.
Saccades
Rapid eye movements
between targets depend on
intact brainstem burst neurons and frontal lobe planning. Latency, velocity, and accuracy abnormalities reveal specific lesion locations.
Vergence
Convergence and divergence
enable depth perception and
near vision. Vergence
insufficiency is epidemic in
digital device users and
creates profound symptoms
that impact daily function.
Gaze Holding
Maintaining stable eye position
requires neural integrator
function. Gaze-evoked
nystagmus and drift patterns
indicate cerebellar pathology
or medication effects.
Optokinetic Nystagmus
OKN responses to moving visual fields test pursuit and saccadic systems simultaneously. Asymmetries indicate hemispheric dysfunction and
help lateralize neurological findings.
Ocular Motor Disorders in Clinical Practice
Every ocular motor disorder represents a specific pattern of neural
dysfunction. Learning to recognize these patterns enables precise
diagnosis and targeted intervention. This module trains you to identify
the most clinically relevant abnormalities and understand their
neurological implications.
You’ll develop systematic approaches to examination that reliably detect
dysfunction, even in subtle presentations. More importantly, you’ll learn
how these findings correlate with patient symptoms and functional
limitations, enabling you to predict which interventions will produce the
greatest clinical impact.
Vergence Insufficiency
Inability to maintain convergence at near
distances. Creates eye strain, headaches,
double vision, and reading difficulties.
Present in 70% of post-concussion
patients and increasing among digital
device users.
Pursuit Deficits
Jerky tracking movements with corrective saccades. Indicates cerebellar or parieto- occipital dysfunction. Correlates with balance problems, motion sensitivity, and difficulty with moving environments.
Saccadic Abnormalities
Altered latency, velocity, or accuracy of rapid eye movements. Hypometric saccades suggest cerebellar pathology; hypermetric saccades indicate different cerebellar regions. Latency changes reveal cortical processing deficits.
Gaze-Holding Failure
Inability to maintain stable eye position in
eccentric gaze. Produces nystagmus,
oscillopsia, and visual blurring. Classic
finding in cerebellar disorders and certain
medication toxicities.
OKN Asymmetries
Unequal optokinetic responses in different
directions. Strongly lateralizes cortical or
brainstem lesions. Useful for
differentiating peripheral from central
causes of dizziness and imbalance.
Visual-Vestibular-Postural Integration
Eye movements do not exist in isolation — they form part of an integrated sensorimotor network that maintains spatial orientation, postural stability,
and coordinated movement. Understanding this integration is essential for clinical application.
The vestibulo-ocular reflex (VOR) stabilizes gaze during head movement through direct connections between the vestibular system and ocular motor
nuclei. When VOR function is compromised, patients develop compensatory strategies that often create secondary problems including neck pain,
postural asymmetries, and movement restrictions.
Visual input powerfully influences muscle tone throughout the body. Abnormal eye movements create tonic asymmetries that perpetuate dysfunction
even when the primary injury has healed. Manual practitioners who address these visual-postural relationships achieve superior outcomes in cases
that have failed conventional treatment approaches.

Visual Input
Retinal signals processed through cortical
pathways
Central Integration
Cerebellum coordinates visual, vestibular,
and proprioceptive information
Motor Output
Influences eye position, neck tone, and
postural control simultaneously
What You Will Master
Complete Anatomical Understanding
Master extraocular muscle anatomy, cranial nerve pathways,
brainstem nuclei, cerebellar circuits, and cortical control regions. Understand how each component contributes to normal and
abnormal eye movements.
Clinical Examination Protocols
Perform systematic assessment of all five eye movement types with reliability and precision. Develop observational skills that
detect subtle abnormalities others miss.
Diagnostic Decision-Making
Interpret findings within neurological frameworks. Differentiate peripheral from central causes, lateralize lesions, and determine
which dysfunctions require priority intervention based on
clinical presentation.
Integration Principles
Understand visual-vestibular-postural relationships that
influence treatment outcomes. Recognize how ocular
dysfunction perpetuates musculoskeletal complaints and limits rehabilitation progress.
Rehabilitation Strategies
Apply evidence-based ocular rehabilitation protocols that
enhance manual therapy outcomes. Design progressive
treatment plans that restore normal eye movement function and eliminate compensatory patterns.
Clinical Communication
Document findings professionally and communicate with
medical specialists using appropriate terminology. Justify
clinical decisions with neurological reasoning that demonstrates advanced expertise.
Transform Your Diagnostic Precision Module 3
Module 3 represents a paradigm shift in how manual practitioners approach
neurological examination. The skills you develop here will distinguish you as an
advanced clinician who thinks and practices at a level that commands
professional respect.
Your patients deserve practitioners who can identify the true drivers of their
symptoms. Your profession deserves practitioners who elevate clinical
standards through mastery of applied neuroscience. You deserve the
confidence that comes from possessing genuine expertise.
Limited enrollment ensures optimal learning conditions and individual attention.
Spaces fill quickly for this advanced module.
Secure Your Place
Join the select group of practitioners who will master ocular
motor assessment and intervention.
Questions about the program? Contact our enrollment team for detailed
information about curriculum, scheduling, and prerequisites.