The Vestibular System: From Theory to Application in Clinical Neuroscience
The Foundation of Posture, Balance, and Human Movement

Master the System That Shapes Human Orientation
The vestibular system is the architect of posture, balance, and spatial awareness —
learn to influence it with precision and confidence. Most clinicians treat the
consequences of vestibular dysfunction, addressing symptoms as they manifest.
NeuroVirtus practitioners treat the source, diving deep into the neurological foundations
that drive human movement and stability.
Module 2 reveals the vestibular system as the hidden driver behind chronic pain,
postural asymmetry, dizziness, and movement inefficiency. This comprehensive training
teaches you how to evaluate and rehabilitate vestibular dysfunction with clinical
authority, transforming your ability to address complex patient presentations that have
frustrated conventional approaches.
The NeuroVirtus Difference
You will learn to see the vestibular system not as a
specialty, but as the foundation of every patient’s
movement, balance, and neurological integrity. This
paradigm shift will fundamentally change how you
approach clinical assessment and treatment planning.

Why This Module Matters
Vestibular dysfunction is often misdiagnosed or overlooked in clinical practice, yet it profoundly influences musculoskeletal presentations across every patient population. The vestibular system doesn’t operate in isolation — it forms the neurological cornerstone of postural control, gaze stability, and spatial orientation. When vestibular function is compromised, the entire kinetic chain adapts, creating compensatory patterns that manifest as pain, asymmetry, and movement dysfunction.
Practitioners who master vestibular assessment gain a powerful advantage in treating complex cases that resist traditional interventions. This module provides the clinical framework to identify vestibular contributions to chronic conditions, differentiate between peripheral and central pathologies, and implement targeted rehabilitation strategies that address the root cause rather than superficial symptoms.
Cerebellar & Vestibular Integration
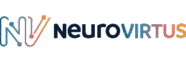
Structural Foundations
Understanding the cerebellum’s architectural organization is essential
for clinical reasoning. You’ll explore the functional divisions of the
cerebellar hemispheres, vermis, and flocculonodular lobe, learning how
each region contributes to motor control, balance, and vestibular
processing.
The deep cerebellar nuclei — dentate, interposed, and fastigial — serve
as critical relay stations that integrate sensory input and coordinate
motor output. Mastering these pathways enables precise localization of
dysfunction.
Neural Circuitry
The cerebellar cortex processes vast amounts of sensory information
through parallel fiber and climbing fiber systems. You’ll learn how
afferent pathways from the vestibular organs, proprioceptors, and visual
system converge on cerebellar circuits.
Efferent projections to the vestibular nuclei, reticular formation, and
motor cortex create the feedback loops that enable real-time postural
adjustments and coordinated movement. Understanding these
connections is fundamental to clinical application.
Vestibular Physiology & Clinical Expression
Semicircular Canals
The three semicircular canals detect angular
acceleration in all planes of head movement.
Each canal contains endolymph and sensory
hair cells that respond to rotational forces.
Understanding canal plane orientation is critical
for interpreting nystagmus patterns and
performing canalith repositioning maneuvers.
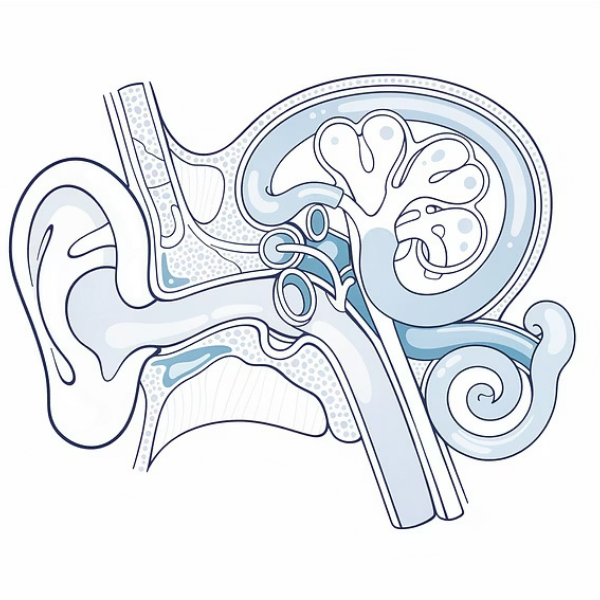
Otolith Organs
The utricle and saccule detect linear
acceleration and head position relative to
gravity. Otoconia crystals embedded in the
gelatinous membrane respond to gravitational
forces, providing essential information for
postural control and spatial orientation.
Dysfunction here creates profound balance
impairment.
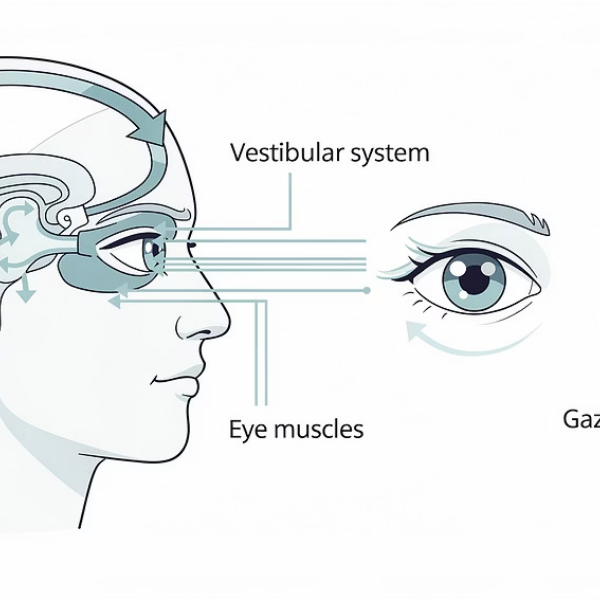
VOR & Gaze Stabilization
The vestibulo-ocular reflex enables clear vision
during head movement by generating
compensatory eye movements. This threeneuron arc operates with remarkable speed and precision. Clinical testing of VOR gain, symmetry, and cancellation reveals critical information about vestibular function and central integration.
Diagnosing Vestibular Dysfunction
Clinical mastery requires the ability to differentiate between diverse vestibular pathologies through systematic examination and pattern recognition.
This module provides the diagnostic framework to confidently identify and classify vestibular disorders based on presentation, nystagmus
characteristics, and functional testing.
Peripheral vs. Central Nystagmus
Learn to distinguish peripheral vestibular lesions from central
pathologies through nystagmus direction, fixation suppression, and
associated symptoms. Central patterns often indicate brainstem or
cerebellar involvement requiring different management strategies.
BPPV Variants
Master the identification and treatment of posterior, horizontal, and
anterior canal BPPV, including canalithiasis and cupulolithiasis
variants. Each presentation requires specific positional testing and
targeted repositioning maneuvers for optimal outcomes.
Vestibular Neuronitis & Labyrinthitis
Differentiate acute vestibular syndrome presentations based on
hearing involvement, symptom onset, and recovery patterns.
Understanding these inflammatory conditions guides appropriate
acute management and rehabilitation timing.
Complex Vestibular Syndromes
Explore superior canal dehiscence, mal de débarquement syndrome,
and oscillopsia. These challenging conditions require sophisticated
clinical reasoning and individualized treatment approaches based on
underlying pathophysiology.
Vestibular-Driven Postural Patterns
The Vestibular-Cervical-Ocular Triad
Vestibular asymmetry doesn’t exist in isolation — it creates predictable compensatory patterns throughout the entire postural system. When one
vestibular organ underperforms, the nervous system adapts by altering cervical mechanics, ocular alignment, and spinal positioning to maintain
functional stability. These adaptations, while initially protective, become maladaptive over time, contributing to chronic pain, restricted motion, and
progressive dysfunction.
Understanding how vestibular asymmetry shapes spinal mechanics is essential for treating stubborn postural presentations. Patients with unilateral
vestibular weakness often demonstrate ipsilateral head tilt, contralateral weight shift, and compensatory cervical rotation. The visual system attempts
to maintain horizontal gaze through ocular counter-rolling, creating additional strain on the oculomotor system.
Vestibular Input
Asymmetric signaling from labyrinth
Central Processing
Brainstem and cerebellar adaptation
Postural Output
Compensatory spinal patterns emerge
What Practitioners Will Gain
Diagnostic Precision
Develop the ability to
differentiate dizziness, vertigo, oscillopsia, and BPPV through
systematic examination and
clinical reasoning. You’ll gain confidence in distinguishing peripheral from central pathologies and identifying specific vestibular syndromes.
Anatomical Mastery
Achieve a deep understanding of cerebellar and vestibular anatomy, physiology, and functional integration. This foundational knowledge enables precise localization of dysfunction and targeted intervention strategies.
Clinical Skills
Learn hands-on skills for
vestibular testing, nystagmus
interpretation, and evidence based rehabilitation protocols. Practice maneuvers and techniques that produce immediate clinical results with appropriate patient populations.
Advanced Reasoning
Develop clinical reasoning
frameworks for vestibulardriven
postural and spinal
dysfunction. Learn to identify
vestibular contributions to
chronic pain and movement
disorders that resist
conventional treatment
approaches.
Rehabilitation Protocols
Master protocols for rebalancing vestibular asymmetries and improving patient stability through progressive challenge and adaptation. Implement strategies that address the neurological foundation of balance disorders.
What You Will Be Able to Do
1. Perform High-Yield Vestibular Testing
Execute comprehensive vestibular and cerebellar examinations
with confidence and precision, including Dix-Hallpike, head
impulse test, dynamic visual acuity, and cerebellar function
screens.
2. Differentiate Complex Presentations
Accurately distinguish between dizziness, vertigo, disequilibrium,
and oscillopsia based on patient history, symptom
characteristics, and objective findings.
3. Apply Targeted Interventions
Implement rebalancing maneuvers, canalith repositioning
techniques, and progressive vestibular rehabilitation protocols
tailored to individual patient presentations and functional goals.
4. Integrate Clinical Findings
Synthesize vestibular assessment findings into comprehensive
treatment plans that address postural asymmetry, manual
therapy sequencing, and movement rehabilitation for optimal
patient outcomes.
Elevate Your Clinical Precision
Limited Enrollment Now Open
Module 2 represents a transformative opportunity to master the
vestibular system and expand your clinical capabilities. This advanced training is designed for practitioners committed to clinical excellence and ready to address the complex neurological foundations of human movement and balance.
Space is intentionally limited to ensure individualized instruction, hands-on practice, and meaningful clinical integration. Reserve your seat in thishigh-impact module and join a community of practitioners dedicated to advancing the field of clinical neuroscience.
Module Details
- 25 hours of intensive training
- Hands-on clinical practice
- Expert faculty instruction
- Comprehensive course materials
- Continuing education credits